This article is evidence-based, verified by Dr. Alexandra Vilceanu MD .
.
Insomnia is one of the most frequent issues in the general population, yet not fully understood and often under-appreciated. Although it has no apparent ‘cure,’ various therapeutic options exist. Treating insomnia becomes a matter of finding the right therapy for the right patient.
An emerging form of psychotherapy, EMDR (Eye Movement Desensitization and Reprocessing), may bring benefits for insomniacs. Preliminary studies suggest its effects are comparable to traditional treatments, while also potentially long-lasting. Its role in clinical practice is yet to be determined.
Medical Disclaimer: The information and recommendations on our site do not constitute a medical consultation. See a certified medical professional for diagnosis.
Sleep
A typical night of sleep consists of 5 stages that repeat cyclically. Stages 1-4 comprise non-REM (non-rapid eye movement) sleep, while stage 5 is REM (rapid eye movement).
Non-REM sleep makes the transition from wakefulness to deep sleep. During this time, we consolidate recollections of the day, committing some to long-term memory. Dreams during this stage are rather plain and based on the day’s experiences.
During REM sleep, the eyes dart back and forth, thus giving this stage its name. During this stage, we experience vivid dreams, while we lose all muscle tone and the body temperature drops.
An EEG recorded during REM state is remarkably similar to one taken while awake, with significant activity throughout the brain and particularly within the hippocampus. From a psychological perspective, REM sleep is thought to play an essential role in processing and consolidating emotional memories .
.
More recent research suggests that REM sleep plays a role in emotional modulation as well. So much so that several studies associate an unusual REM sleep pattern with mood disorders – depression with an increased amount of REM sleep, anxiety with a reduced amount of REM sleep, or PTSD with flashbacks during REM sleep .
.
Insomnia
Insomnia is defined by dissatisfaction with either sleep quantity or quality. Patients experience trouble either falling asleep or maintaining sleep. People with insomnia often only get a few hours of sleep a night, either sleeping late, waking up abnormally early, or both.
Additionally, even if the sleep is of typical duration, it can be of poor quality – nonrestorative sleep being a common complaint among insomniacs. As a consequence, daily activities are invariably affected. Patients experience fatigue, mood swings, and attention deficits.
From a medical perspective, a few types of insomnia can be diagnosed:4
- Acute/ short-term insomnia – symptoms lasting less than three months
- Persistent insomnia – symptoms lasting for three months or longer
- Recurrent insomnia – two or more episodes of insomnia (lasting between 1 and 3 months) over one year
It can be an independent affliction, but it often occurs in the context of another mental disorder – such as anxiety, major depressive disorder, or post-traumatic stress disorder. It is not uncommon that it accompanies medical conditions , such as chronic pain, neurodegenerative diseases, or a breathing-related sleep disturbance.
, such as chronic pain, neurodegenerative diseases, or a breathing-related sleep disturbance.
Chronic insomnia symptoms are estimated to occur in about one-third of adults, although only 6-10% meet the criteria for insomnia disorder. Acute insomnia, however, is estimated to affect as much as 50% of the population .
.
Its long-term consequences range past the patients’ complaints. The chronic lack of proper restorative sleep has been associated with several medical conditions, including hypertension, diabetes, heart disease, arthritis, and chronic pain.
range past the patients’ complaints. The chronic lack of proper restorative sleep has been associated with several medical conditions, including hypertension, diabetes, heart disease, arthritis, and chronic pain.
Treating insomnia
Psychotherapy for insomnia
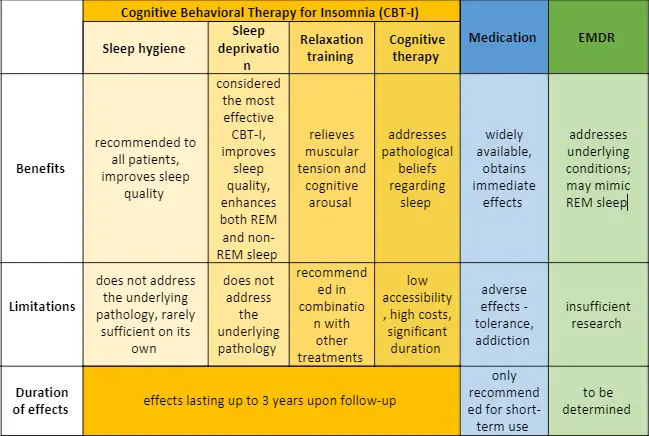
Cognitive-behavioral interventions for insomnia (CBT-I) are considered first-line therapy for insomnia. They are superior to medication in both efficacy and duration of effects and preferred by patients. CBT-I has been shown to enhance both REM and non-REM stages of sleep, improving sleep regulation.
It is of use not only for ischemia alone but also when it presents in the context of other pathologies, including chronic pain, arthritis, migraine, depression, or PTSD. Studies have also shown that CBT-I exerts long-lasting effects, persistent up to 3 years of follow-up.
Cognitive-behavioral interventions include:
Sleep hygiene
The first step in addressing insomnia is putting a set of sleep hygiene recommendations into place. These may include creating a regular sleep schedule, avoiding stimulants like coffee and nicotine, or keeping a dark and quiet bedroom.
The stimulus control portion of sleep hygiene includes techniques such as: always going to bed when sleepy, using the bedroom for sleep alone, avoiding reading or television before sleep, leaving the bed whenever unable to fall asleep, avoiding naps.
Exercise is also an essential part of sleep hygiene recommendations, being proven to improve sleep quality.
Sleep restriction
Although potentially counter-intuitive, limiting the amount of time spent in bed leads to a mild degree of sleep deprivation, subsequently increasing the body’s need for sleep.
As a result, the relatively reduced amount of sleep ends up being of better quality and proves more restful. Sleep restriction is considered the most effective component of CBT-I.
Relaxation training for insomnia
Relaxation training includes methods for relieving muscular tension and cognitive arousal. Classical approaches include progressive muscle relaxation, guided imagery, or breathing techniques.
Recently, mindfulness meditation emerged as a complementary therapeutic intervention aimed at focusing on awareness and attention on the present moment to relax the mind. It has been proven to help reduce dysfunctional beliefs about sleep and combine well with other therapies, including medication.
Cognitive behavioral therapy for insomnia
In a more classical psychological approach, cognitive therapy aims to identify dysfunctional beliefs and attitudes towards sleep and replace them. Techniques may include challenging unhelpful beliefs, journaling, and behavioral ‘experiments’ to test specific assumptions regarding sleep.
Ultimately, CBT-I combines the interventions above in a multimodal treatment catered for the patient’s needs. The main issues CBT-I faces are their accessibility, as they require clinicians with specific training, and cost. As a consequence, a significant proportion of patients is not able to benefit from it.
Medication for insomnia
Pharmacological approaches play an indisputable role in insomnia management as well. Benzodiazepines are the main class of interest here, being employed as an insomnia treatment for the past 30 years.
They act by enhancing the effect GABA (γ-aminobutyric acid) has on the brain as the primary inhibitory neurotransmitter.
While their efficacy is apparent, they are only recommended in short-term regimens, and especially for acute insomnia. Long-term use is associated with a significant risk of tolerance and addiction, and, although controversially, with higher overall mortality.
In the past years, alternatives to benzodiazepines have been proposed as options with better efficacy and fewer side effects. An exciting new prospect is Suvorexant, which addresses a different signaling pathway in the brain, responsible for waking up.
So far, it produced encouraging safety and efficacy results in clinical trials.
Other medications, such as melatonin, anti-histamines, or anti-depressants, may also be employed in an insomnia treatment scheme. Despite all efforts, as many as 40% of chronic insomnia patients cannot achieve sustained results.
What is EMDR?
EMDR – short for Eye Movement Desensitization and Reprocessing is an emerging form of psychotherapy, pioneered in 1987 by Francine Shapiro.
It was initially designed to help patients manage traumatic events. During sessions, patients would recall brief instances of the traumatic event, while at the same time performing a distracting action.
Most commonly, this would be lateral eye movements dictated by the therapist – hence the name. Nevertheless, a variety of other external stimuli can be used, such as hand-tapping or listening to a particular sound.
The scope of this form of therapy is that the patient accesses the traumatic event and processes it, ultimately gaining a type of adaptive behavior to the distressing recollection.
The external stimulus – be it eye movement or another – is to maintain the patient simultaneously focused on both the memory and an element of the outside world.
The World Health Organization recognized EMDR as an appropriate form of psychotherapy for PTSD in children, teenagers, and adults in 2013. Its use is currently expanding to other health conditions, including psychosis, bipolar disorder, depression, anxiety disorders, substance abuse disorders, and chronic back pain .
.
EMDR relies on the Adaptive Information Processing Model. This assumes that much of psychopathology is based on improper encoding or processing of traumatic events.
Therapist-guided eye movements should help overcome the reticence in accessing the memory and anchor the subject in the present moment as he processes and re-encodes the event.
Can EMDR Treat Insomnia?
Two main arguments suggest EMDR may bring benefits to insomniacs: addressing the underlying affliction that causes insomnia and creating a REM-like state during sessions.
EMDR for underlying afflictions
As stated before, insomnia is often a manifestation of another underlying pathology. PTSD, anxiety, and depression can all associate insomnia symptoms. In these situations, treating the cause is the optimal course of action.
EMDR therapy has been proven at least equally effective as other forms of psychotherapy in PTSD, sometimes with faster results and better tolerance from patients. Guidelines include using EMDR in PTSD as a strong recommendation, as it improves both clinical symptoms and quality of life.
EMDR has also demonstrated positive preliminary results in clinical trials for depression, anxiety and obsessive-compulsive disorders, chronic pain, and possibly even psychotic disorders.
in clinical trials for depression, anxiety and obsessive-compulsive disorders, chronic pain, and possibly even psychotic disorders.
All these pathologies may associate insomnia, which could, in turn, be alleviated upon treating the condition itself.
Research assessing the improvements EMDR brings to sleep alone in psychiatric conditions is not as abundant. One 2014 study evaluates the effects EMDR has on mood, anxiety, subjective and objective sleep on a small sample of 13 PTSD patients versus controls.
Polysomnographic data shows that, after 3-10 sessions, patients experienced more consolidated sleep and reduced time spent awake after sleep onset.
Interestingly, another study assesses the effect EMDR has on insomnia severity in patients with rheumatoid arthritis and compares it with guided imagery (a form of relaxation training, part of the CBT-I).
and compares it with guided imagery (a form of relaxation training, part of the CBT-I).
Both techniques reduced insomnia in patients compared to controls, but the EMDR group experienced a more significant alleviation.
EMDR and REM sleep
There is a certain resemblance between the aspect of an EMDR session and REM sleep – both involve recollecting emotionally-rich situations while tending to some external stimulus, often enough eye movements.
This raises the question as to whether EMDR may bring some of the REM sleep benefits, or help with the chronic REM sleep deprivation.
A set of neuroimaging findings supports this hypothesis. EMDR sessions seem to change and consolidate how memory is processed much in the way REM sleep does.
Furthermore, emotional processing appeared to be enhanced, reminiscent of emotional memory processing during REM sleep.
Other neurobiological resemblances have been noted, such as the increased activity in the amygdala, medial prefrontal cortex, and hippocampus in both EMDR and REM sleep. These regions are involved in emotional processing and regulation, as well as learning and memory.
EEG data collected during EMDR sessions are similar to slow-wave sleep, supposedly prompting memory integration and inducing a sense of relaxation and safety.
EMDR’s role in insomnia therapy
The longevity of EMDR effects is still being debated, as research on the issue relies mainly on small clinical studies. Nevertheless, several papers reported that a proper EMDR therapy course, including all necessary sessions, can lead to lasting effects at three months, six months, and even 35 months of follow-up.
This would make it comparable to other CBT-I interventions.
Despite promising preliminary observations, more large-scale, randomized controlled trials are required to accurately assess EMDR’s efficacy as a therapeutic tool in insomnia, both as a stand-alone and other methods.
In a Position Paper, the American Academy of Sleep Medicine includes EMDR as a therapeutic tool that may be used for the treatment of PTSD-associated nightmares.
Final Thoughts
To sum up, insomnia has a significant impact on the quality of life and should be adequately addressed. In addition to the daily grogginess and exhaustion, depriving the brain and the whole body of a restoring night of sleep can have significantly detrimental effects.
When insomnia has a clear cause, such as a traumatic event, anxiety, or a different underlying psychological condition, treating the ailment is the preferred course of action for lasting effects.
EMDR may come into play here, with its proven results on trauma management.
Nevertheless, due to the therapy’s unique resemblance to REM states of sleep, its benefits may range past this classical indication and aid other forms of sleep disturbances.
Large-scale studies are required to confirm its benefits, accurately compare it to other treatment options, and determine its place in medical practice.
How Effective Is Yoga For Insomnia?

Alexandra Vilceanu graduated in medicine from Carol Davila University of Medicine and Pharmacy, Bucharest. During her studies, she had a particular interest in research. She spent a significant amount of time in the cell biology laboratory from Victor Babeș Institute of Pathology, Bucharest. She was also an active member of the Scientific Organization for Medical Students (SOMS), and a founding member of the SOMS Molecular department. Alexandra is a rising star, and her career will continue at the Institute of Molecular Pathology, Vienna, studying neurodevelopmental anomalies.
graduated in medicine from Carol Davila University of Medicine and Pharmacy, Bucharest. During her studies, she had a particular interest in research. She spent a significant amount of time in the cell biology laboratory from Victor Babeș Institute of Pathology, Bucharest. She was also an active member of the Scientific Organization for Medical Students (SOMS), and a founding member of the SOMS Molecular department. Alexandra is a rising star, and her career will continue at the Institute of Molecular Pathology, Vienna, studying neurodevelopmental anomalies.
References
- Buysse, D. J. Insomnia. JAMA – Journal of the American Medical Association 309, 706–716 (2013).
- Kandel, E., Schwartz, J., Jessell, T., Siegelbaum, S. & Hudspeth, A. J. Principles of Neural Science. (Elsevier, 2012)
 .
. - Hutchison, I. C. & Rathore, S. The role of REM sleep theta activity in emotional memory. Frontiers in Psychology 6, 1439 (2015).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition – DSM V. Psychopathology and Psychotherapy: DSM-5 Diagnosis, Case Conceptualization, and Treatment (2013). doi:10.4324/9780203772287-23
- Riemann, D. et al. The neurobiology, investigation, and treatment of chronic insomnia. The Lancet Neurology 14, 547–558 (2015).
- Medic, G., Wille, M. & Hemels, M. E. H. Short- and long-term health consequences of sleep disruption. Nature and Science of Sleep 9, 151–161 (2017).
- Kay-Stacey, M. & Attarian, H. Advances in the management of chronic insomnia. BMJ (Online) 354, (2016).
- Eye Movement Desensitization and Reprocessing (EMDR) Therapy. Available at: https://www.apa.org/ptsd-guideline/treatments/eye-movement-reprocessing
 . (Accessed: 24th August 2020)
. (Accessed: 24th August 2020) - Valiente-Gómez, A. et al. EMDR beyond PTSD: A Systematic Literature Review. Front. Psychol. 8, 1668 (2017).
- Novo Navarro, P. et al. 25 years of Eye Movement Desensitization and Reprocessing (EMDR): The EMDR therapy protocol, hypotheses of its mechanism of action, and a systematic review of its efficacy in the treatment of post-traumatic stress disorder
 . Rev. Psiquiatr. y Salud Ment. (English Ed. 11, 101–114 (2018).
. Rev. Psiquiatr. y Salud Ment. (English Ed. 11, 101–114 (2018). - Chamberlin, D. E. The Predictive Processing Model of EMDR
 . Front. Psychol. 10, 4 (2019).
. Front. Psychol. 10, 4 (2019). - Raboni, M. R., Alonso, F. F. D., Tufik, S. & Suchecki, D. Improvement of mood and sleep alterations in posttraumatic stress disorder patients by eye movement desensitization and reprocessing.
 Front. Behav. Neurosci. 8, (2014).
Front. Behav. Neurosci. 8, (2014). - Ghanbari, N., Afrasiabifar, N. A. & Cooper, R. Z. The Effect of EMDR Versus Guided Imagery on Insomnia Severity in Patients With Rheumatoid Arthritis. (2019)
 . doi:10.1891/1933-3196.13.1.2
. doi:10.1891/1933-3196.13.1.2 - Stickgold, R. Sleep-Dependent Memory Processing, and EMDR Action
 . J. EMDR Pract. Res. 2, 289–299 (2008).
. J. EMDR Pract. Res. 2, 289–299 (2008). - Carletto, S., Borsato, T. & Pagani, M. The Role of Slow Wave Sleep in Memory Pathophysiology: Focus on Post-traumatic Stress Disorder and Eye Movement Desensitization and Reprocessing
 . Front. Psychol. 8, 2050 (2017).
. Front. Psychol. 8, 2050 (2017). - Pagani, M., Amann, B. L., Landin-Romero, R. & Carletto, S. Eye movement desensitization and reprocessing and slow-wave sleep: A putative mechanism of action
 . Front. Psychol. 8, (2017).
. Front. Psychol. 8, (2017). - Morgenthaler, T. I. et al. Position paper for the treatment of nightmare disorder in adults: An American Academy of sleep medicine position paper. J. Clin. Sleep Med. 14, 1041–1055 (2018).